Although Prostate cancer surgery has undoubtedly improved over the past two decades with experienced surgeons and robot-assisted surgery, men are still rightly concerned about the twin threats of incontinence and impotence; here, with expert surgeon Christopher Eden, we explore this.
1. An experienced surgeon is crucial; keyhole surgery
Christopher Eden is a Consultant Urologist at The Royal Surrey County Hospital in Guildford and director of The Prostate Clinic, based at The Hampshire Clinic in Old Basing, Hampshire. He is the pioneer of laparoscopic (keyhole) radical prostatectomy in the UK and has the country's greatest experience of laparoscopic surgery on the urinary tract, having completed 2,000 cases. He performs approximately 250 laparoscopic urological operations each year. At icon, a decade ago, we asked him to write this piece following an article in the National Press which concluded that the risks of side effects when having prostate surgery diminished, the greater the experience of the surgeon.

Christopher Eden
www.theprostateclinic.com
Patients who have just received a diagnosis of localized prostate cancer are often sent away with literature about the several possible ways of treating their condition and usually face a difficult time navigating their way through the pros and cons of each treatment. However, although several choices are available to most patients, not all choices are equal.
Radical prostatectomy (RP) for localised and locally advanced prostate cancer is associated with a unique set of advantages over its alternative treatment options: it is the most successful treatment for organ-confined prostate cancer (1) and is the only treatment for localized prostate cancer that has shown a cancer-specific survival benefit in a prospective, randomised trial (2) . It offers suitable patients not only good functional results (erections and continence) and cancer control but also early detection of cancer recurrence (indicated by a measurable PSA) and the strong safety net of radiotherapy when appropriate. Why then are patients drawn to newer techniques, such as brachytherapy, cryotherapy and HIFU, which lack mature results, or to focal therapy for what is a multifocal disease in 80 per cent of patients?

Multifocal prostate cancer (red); all 15 biopsies from the left lobe were negative
Although the concept of RP is simple (removing the prostate and joining the cut ends of bladder and urethra together) its practice is not simple due to its location deep in the narrow male pelvis beneath the pubic bone, the crowding together of vital structures around it, its excellent blood supply and the variation in prostate anatomy between patients. No surprise, then, that although radical prostatectomy was first performed in 1902 it failed to achieve popularity amongst surgeons (let alone their patients) until after 1982, when Walsh and Donker published their research detailing the blood and nerve supply of the prostate (3) . For the first time this allowed the operation to be performed with acceptable blood loss and with an expectation of continence and erections after surgery.
Since that time several North American centres (Johns Hopkins Hospital in Baltimore, the Mayo Clinic in Rochester and Memorial Sloane Kettering Hospital in New York, in no particular order) have published the results of large RP series and have made their reputations chiefly through this one operation. In turn, surgeons around the world have recommended RP to their patients, citing the excellent results from these institutions, but have often failed to achieve results that even come close to those from across the Atlantic themselves. Why has this been so? A glance at the table below provides the explanation.
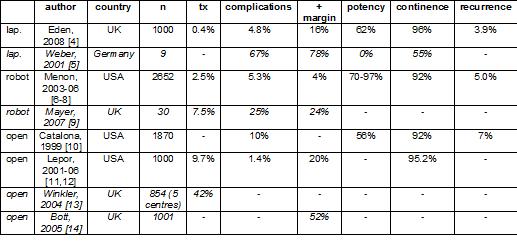
The best and the worst (italics) results of radical prostatectomy. lap. = laparoscopic; n = number of patients; tx = blood transfusion; + margin = positive surgical margins (world-class results are considered to be less than 20%); - = not stated.
The table shows that the common denominator for excellent results from RP is not the method used to perform the operation, or what continent it is done in, but surgical experience. This message is intuitively correct but proof has only been available for the past few years, during which time the evidence has rapidly accumulated. The link between high surgical volume and improved patient outcomes has been established for many complicated operations (surgery on the pancreas and oesophagus, for instance) and this list now includes radical prostatectomy (15, 16) . Although hospital volume is also important, it is the surgeons individual volume that is more important in determining the patients outcome (17) . In fact, the only determinants of patient outcome following RP (apart from chance) appear to be the cancer parameters (tumour grade & stage and PSA), which are fixed, and the person doing the operation.
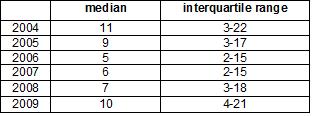
The Calman/Hine report in 1995 recognised the importance of concentrating cancer treatment into fewer centres and formed the basis of the current governments radical re-organisation of cancer services in the UK in 2000 in the form of their Cancer Plan, detailed in NICEs publication Improving Outcomes Guidance (IOG). The aim of IOG was to drive complex operations into fewer, larger centres, so promoting sub-specialisation amongst surgeons and improving results. The process in the UK to date has been patchy and slow but the table below illustrates that progress is gradually being made.
Table. Annual individual surgeon caseload for RP in the UK (18)
If you or one of your friends or family are unlucky enough to have prostate cancer diagnosed, you should ask your urologist to discuss with you all the treatments you are suitable for and to explain why you are unsuitable for the remainder. You should ask about the advantages and disadvantages of each and you should ask for a recommendation on exactly what the urologist thinks is the best treatment and why. Finally, you should ask how many cases he or she does a year and about their results. Do not be afraid to get a second opinion if you think you need one. Good luck! Christopher Eden
2. Robotic Surgery - what is it?
The most common type of surgery for prostate cancer is a Radical Prostatectomy, where the surgeon removes the prostate gland and some tissue around the outside - such as the seminal vesicles.
As Christopher says above, rather than making a cut from the navel downwards, keyhole surgery seems much less invasive. This keyhole surgery may also involve a robotis system - robotic-assisted laparoscopic radical prostatectomy, or Robotic Prostatectomy, or Robotic surgery. The surgeon sits at a control panel and moves robotic arms through the several small incisions. It is still keyhole surgery.
Robotic keyhole surgery means less blood loss, pain, and a faster recovery time. But, in truth, according to the American Cancer Society, Robotic Surgery seems to make little difference when it comes to urinary or erection problems.
Go to: HFU, ablation, Nanoknife in Prostate cancer
********************************
PEOPLE READING THIS ARTICLE ALSO READ:
Prostate Cancer Overview
Go to: Prostate Cancer - symptoms, causes and treatment alternatives
********************************
References
1. Lu-Yao GL, Yao SL. Population-based study of long-term survival in patients with clinically localised prostate cancer. Lancet 1997; 349: 906-910.
2. Guidelines on prostate cancer. European Association of Urology, 2007. http://www.uroweb.org/filetx_eauguidelines/2001_prostate_cancer.pdf
3. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. Journal of Urology 1982; 128: 492-497.
4. Eden CG, Neill MG, Louie-Johnsun MW. The UKs first 1,000 cases of laparoscopic radical prostatectomy: evidence of multiple learning curves. British Journal of Urology International 2008 (in press).
5. Weber HM, Eschholz G, Gunnewig M, Krah XA, Benken N. Laparoscopic radical prostatectomy?-not for us! Journal of Urology 2001; 165: 616A.
6. Menon M, Tewari A, Peabody J. Vattikuti Institute Prostatectomy: Technique. Journal of Urology 2003; 169: 2289-2292.
7. Kaul S, Savera A, Badani K, Fumo M, Bhandari A, Menon M. Functional outcomes and oncological efficacy of Vattikuti Institute prostatectomy with Veil of Aphrodite nerve-sparing: an analysis of 154 consecutive patients. British Journal of Urology International 2006; 97: 467-472.
8. Menon M, Shrivastava A, Kaul S et al. Vattikuti Institute Prostatectomy: contemporary technique and analysis of results. European Urology 2007; 51: 648658.
9. Mayer EK; Winkler MH, Undre S, McGregor R, Hrouda D, Ogden C, Karim O, Vale JA. Initial UK experience with robotically assisted laparoscopic radical prostatectomy (RAP) using a team approach. Prostate Cancer & Prostate Disease 2006; 9: 457-458.
10. Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. Journal of Urology 1999; 162: 433-438.
11. Lepor H, Nieder AM, Ferrandino MN. Intraoperative and postoperative complications of radical retropubic prostatectomy on a consecutive series of 1,000 cases. Journal of Urology 2001; 166: 1729-1733.
12. Sultan R, Slova D, Thiel R, Lepor H. Time to return to work and physical activity following open radical retropubic prostatectomy. Journal of Urology 2006; 176: 1420-1423.
13. Winkler MH, Khan FA, Oeke M, Sugiono AA, Bousted GB, Persad R, Kaisary AV, Gillatt DA. PSA to improve case selection for radical prostatectomy in the UK. British Journal of Urology International 2004; 93 (supplement 4): 43.
14. Bott SR, Freeman AA, Stenning S, Cohen J, Parkinson MC. Radical prostatectomy: pathology findings in 1001 cases compared with other major series and over time. British Journal of Urology International 2005; 1: 34-39.
15. Klein EA, Bianco FJ, Serio AM, Eastham JA, Kattan MW et al. Surgeon experience is strongly associated with biochemical recurrence after radical prostatectomy for all preoperative risk categories. Journal of Urology 2008; 179: 2212-2217.
16. Alibhai SM, Leach M, Tomlinson G. Impact of hospital and surgeon volume on mortality and complications after prostatectomy. Journal of Urology 2008; 180: 155-163.
17. Wilt TJ, Shamliyan TA, Taylor BC, MacDonald R, Lane RL. Association between hospital and surgeon radical prostatectomy volume and patient outcomes: a systematic review. Journal of Urology 2008; 180: 820-829.
18. British Association of Urological Surgeons Cancer Registry Publications http://www.sarahfowler.org/endourology.htm